September 2025
Pulmonary alveolar proteinosis with hypersensitivity pneumonitis: A rare case of overlap syndrome.
A 35 year old casual smoker presented three days post-partum with breathlessness. CTPA demonstrated bilateral diffuse ground glass opacification with a mild lower lobe predominance.
In the following years the patient had multiple admissions to hospital with shortness of breath, recurrent cough and haemoptysis. Serial CT imaging demonstrated worsening of the ground glass opacification. This had a lower lobe predominance but there was no interlobular septal thickening.
Symptoms mostly improved with steroids. Further investigations included bronchoscopy, spirometry, and vasculitis screen which were all negative.
A definitive diagnosis remained elusive, and subsequently a surgical lung biopsy was arranged. The patient was also referred to immunology due to lymphopenia, which had features indicating this may be secondary to lymphatic protein loss. There were no clear exposure factors to suggest hypersensitivity pneumonitis, though the patient reported they had recently stopped smoking, which is a known protective factor (1) .
Before the biopsy had been fully analysed, the patient presented with acute exacerbation and was critically unwell. Imaging at this time demonstrated multi-lobar lung collapse. The patient was transferred to a specialist centre for ECMO support and treatment with total lung lavage.
During their extended admission at the quaternary centre the lung biopsy sample was reviewed, and following discussion at the rare diseases MDT a diagnosis of pulmonary alveolar proteinosis with hypersensitivity pneumonitis overlap was made.
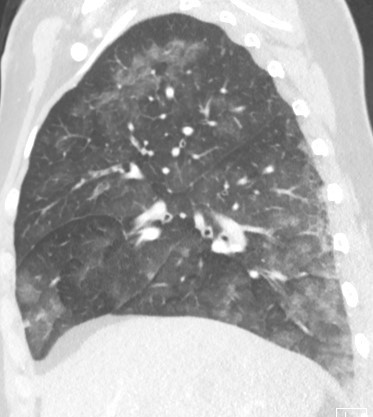
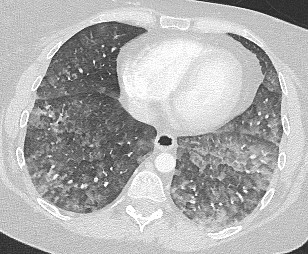
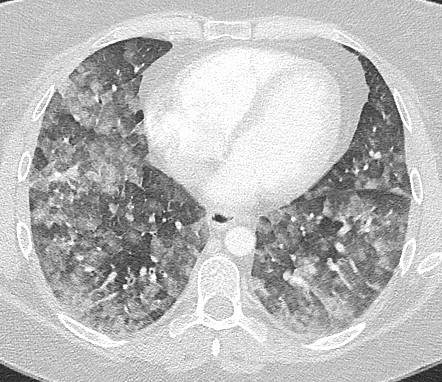

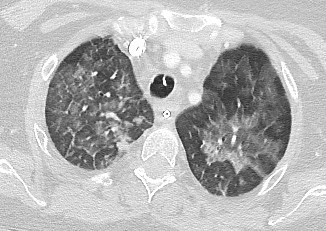
Fig 3 - 7. Progressive increase in ground glass opacification, turning into a crazy paving appearance, with GG centrilobular nodules still seen in the apices.
Discussion
Typical appearances of (non-fibrotic) hypersensitivity pneumonitis is described as ill-defined centrilobular or diffuse ground glass opacification, which is often upper zone predominant. Mosaic attenuation can also be seen with the characteristic ‘three density pattern’ including air trapping, particularly on expiratory phase imaging (2). However, to diagnose HP is it also important to identify an underlying exposure which is causing this reaction. With long term exposure it can also progress into fibrotic HP, with the accompanying signs of peripheral reticulation, traction bronchiectasis, volume loss and honeycombing.
This is quite different to pulmonary alveolar proteinosis (PAP). Whilst both conditions involve ground glass opacification, the characteristic imaging finding with PAP is the crazy paving appearance. This consists of ground glass opacification and interlobular septal thickening, which is also usually lower lobe predominant (3).
In this case the initial CT imaging had patchy GGO throughout both lungs, with a slight lower lobe predominance. Due to the centrilobular distribution of the GGO, initial reports raised HP as the most likely differential. The GGO progressed over many years but did not demonstrate the typical ‘crazy paving’ appearance typical of PAP until 5 years later, after the biopsy had already made the diagnosis.
On later imaging, the characteristic crazy paving appearance of PAP was accompanied by persistent ground glass centrilobular nodules in the upper lobes.
PAP and HP are both distinct pathologies with varying features on imaging. However, when co-existing these features have been described as an overlap syndrome (4). It has also been hypothesised that these conditions may interact, for example, a hypersensitivity reaction secondary to the PAP lipoproteinacious material.
Conclusion
PAP is a rare condition and in this case presented with atypical features. PAP with HP overlap has features of both conditions and should be considered in patients with imaging findings not typical of one or the other. This case highlights the need to consider multiple interacting pathologies when a diagnosis is proving elusive.
Questions:
- Which of the following statements is false regarding smoking?
- Smoking is a protective factor for hypersensitivity pneumonitis.
- Smoking is strongly associated with pulmonary alveolar proteinosis.
- Smoking is protective for pulmonary alveolar proteinosis.
- There is a male predilection in smokers with pulmonary alveolar proteinosis.
- What is the primary treatment for pulmonary alveolar proteinosis?
- Steroids
- Total lung lavage
- Methotrexate
- Lung transplant
- Which sign is commonly seen in hypersensitivity pneumonitis?
- Crazy paving
- Halo sign
- Head cheese sign
- Bat wing sign
- Which of these is NOT a feature of ‘crazy paving’?
- Ground glass opacities
- Interlobular septal thickening
- Consolidation
- Intralobular septal thickening
Answers:
1: C – smoking is protective for pulmonary alveolar proteinosis.
This is an incorrect statement. Smoking is a protective factor for hypersensitivity pneumonitis, but is strongly associated with PAP.
2: B – total lung lavage is the treatment of choice for PAP.
Total lung lavage is the practice of washing the patients lungs with saline by filling and draining. This removes the surfactant proteins which cause PAP.
3: C – Head cheese sign
The head cheese sign is also known as the three density pattern or three attenuation pattern. This refers to the mosaic appearance with areas of low density (lucent areas of air trapping), medium density (normal lung), and high density (ground glass opacification). This appearance is traditionally associated with hypersensitivity pneumonitis but can also be seen in other conditions, particularly those causing small airway obstruction. Head cheese is a type of terrine composed of pieces of meat scavenged from various parts of various animals.
4: C – Consolidation
Crazy paving is the imaging appearances of a combination of ground glass opacification and both interlobular and intralobular septal thickening.
References
- Blanchet, M.-R., Israël-Assayag, E. and Cormier, Y. (2004). Inhibitory Effect of Nicotine on Experimental Hypersensitivity PneumonitisIn VivoandIn Vitro. American Journal of Respiratory and Critical Care Medicine, [online] 169(8), pp.903–909. doi:https://doi.org/10.1164/rccm.200210-1154oc.
- Magee, A.L., Montner, S.M., Husain, A., Adegunsoye, A., Vij, R. and Chung, J.H. (2016). Imaging of Hypersensitivity Pneumonitis. Radiologic Clinics of North America, 54(6), pp.1033–1046. doi:https://doi.org/10.1016/j.rcl.2016.05.013.
- Holbert, J.M., Costello, P., Li, W., Hoffman, R.M. and Rogers, R.M. (2001). CT Features of Pulmonary Alveolar Proteinosis. American Journal of Roentgenology, 176(5), pp.1287–1294. doi:https://doi.org/10.2214/ajr.176.5.1761287.
- H. Verma, A.G. Nicholson, K.M. Kerr, O.J.Dempsey, A.R. Gibbs, I. Campbell, et al. Alveolar proteinosis with hypersensitivity pneumonitis: a new clinical phenotype. Respirology, 15 (2010), pp. 1197-1202




